Underuse of Appropriate Healthcare is Harmful and Costly
This article about healthcare was adapted from an original post dated July 12, 2018 on www.statnews.com.
The phrase “less is more” has become omnipresent in health care. Whether it’s inserting too many artery-opening stents into people with angina, performing too many surgeries for back pain, ordering too many CT scans for headaches, or prescribing too many narcotics for people with chronic pain, overuse is rampant in our medical system. As the Senate tries to fashion a bill that will likely end up taking away access to health care from millions of Americans, it is important to remember that underuse of evidence-based services is an equally pressing issue. When it comes to health, less is sometimes lesser.
While the United States outspends every other developed nation on healthcare — nearly 18 percent of our gross domestic product — Americans lag behind many other countries in the quality of care they receive at the beginning, middle, and end of their lives. This discordance has increased pressure to reduce costs, and so-called medical waste has become a prominent target. While several measures have been developed to curb wastefulness, some of these have had the unintended consequence of reducing access to potentially lifesaving treatments or therapies.
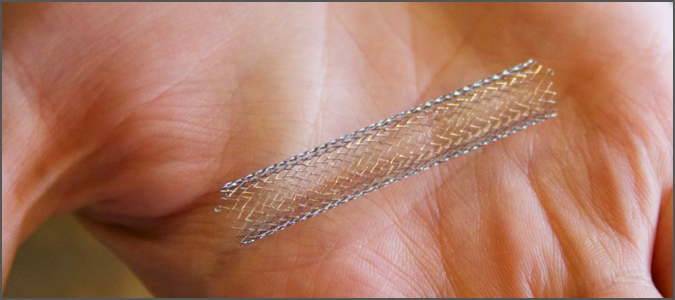
In cardiology, my specialty, the overuse of artery-opening stents has gained substantial attention. While absolutely lifesaving when used for someone in the throes of a heart attack, stents are no better than medication for improving outcomes for patients who have the stable chest pain known as angina. To set standards for stent placement, professional cardiology societies have introduced “appropriateness criteria” that offer guidelines as to when, and when not, to place a stent.
Many states now also require public reporting of patient outcomes after stent placement. While this reporting has helped reduce unnecessary use of stents, it has also led to their underuse in the sickest patients, presumably because physicians did not want to have poorer outcomes and death — which would be expected in this population — “count against them.”
A similar story has evolved in the world of health insurance. In an effort to make consumers more cost-sensitive, insurers have increased copays associated with medical charges. This strategy has had some benefits. “A significant part in the slowdown of heathcare costs is related to patients having more skin in the game,” Dr. Mark McClellan, a former head of the Food and Drug Administration and the Centers for Medicare and Medicaid Services, and now the director of the Margolis Center for Health Policy at Duke University, told me.
However, a clinical trial involving about 6,000 individuals who had just suffered heart attacks showed that those who had no copays associated with their medications had lower rates of future strokes, heart attacks, and other cardiovascular complications, and incurred no increased cost to insurers, compared to those with standard copays. A significant increase in complications among those with copays was driven primarily by fewer patients taking their prescribed medications. African-Americans are especially prone to underusing medications due to cost. In other words, well-meaning policies meant to curb excess can limit access.
Medical interventions aimed at preventing disease or keeping it from escalating are universally underused compared to those with shorter-term effects. Consider people with asthma. It’s recommended that they use a daily “controller” inhaler to ease the airway inflammation at the root of the disease, as well as a “rescue” inhaler that provides only short-term relief when symptoms appear. Yet controller inhalers are widely underused while many individuals with asthma overdose on rescue inhalers.
This is true with regard to heart disease as well: Even as the use of cardiac imaging and cardiac procedures are skyrocketing, inexpensive medications proven to prevent future heart attacks and strokes are inconsistently prescribed or taken. A similar trend is observed in immunization and screening tests.
The low uptake of appropriate medical services can actually lead to downstream overuse. African-Americans, Hispanics, and other minorities are more likely to undergo procedures and surgeries at the end of life and incur significantly more costs in the last six months of life than whites. Much of this is driven by an underuse of preventive measures in the years preceding the end.
A movement toward performance-based payments may increase the use of appropriate care by physicians and health systems. “All services are vulnerable to over- and under-utilization,” Dr. Harlan Krumholz, a cardiologist and professor at Yale University, wrote to me in an email, “and the challenge for the future is to provide the information that helps patients make the best choices.” A stent, for example, can be the most — and least — appropriate intervention for a patient, given the clinical context. Patients need to be more engaged in their health care and their physicians need to balance medical treatments that are less likely to provide instant relief with those that reduce the risk of serious events over the long term.
Over the past decade, some healthcare experts have skeptically asked the question, “Is more care better?” Policymakers mulling the Senate healthcare bill must keep in mind that, when the care is truly appropriate, more is indeed better.
According to the Dartmouth Atlas of Health Care, which has been exploring variations in the use and distribution of medical resources in the United States for the past 20 years, spending decreases when recommended care is practiced.
Too much medicine has been the source of unbridled indignation over the past few years. Curiously, there’s been little outcry about the underuse of evidence-based care. Perhaps this differential reaction stems from the incorrect notion that overuse is associated with rising medical costs while underuse of evidence-based care isn’t. That’s simply not true.
Many studies that have evaluated the number of patients who rightly received specific services did not analyze how many did not get them. So rather than looking at overuse and underuse, perhaps we need to focus on appropriate care, or what the Lown Institute, a Boston-based nonprofit think tank, refers to as RightCare, which melds these two seemingly opposite trends.
Haider Warraich, M.D., is a fellow in cardiology at Duke University Medical Center and the Duke Clinical Research Institute, and author of “Modern Death: How Medicine Changed the End of Life” (St. Martin’s Press).